The Evolution of the Pacemaker: A Conversation with Cardiologist Dr. Abraham Bornstein, M.D., Part I
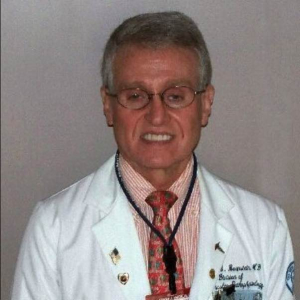
Dr. Abraham B. Bornstein, M.D., F.A.C.C
Dr. Abraham B. Bornstein, M.D., F.A.C.C. is a board-certified interventional and clinical cardiologist. He received his M.D. from Tufts University School of Medicine in 1973 and was assistant professor of medicine at Weill Cornell Medical College, specializing in cardiovascular pathophysiology, pediatric cardiology and adult congenital heart disease. He did a cardiology fellowship at the Tufts-New England Medical Center. Dr. Bornstein has more than 30 years of clinical practice experience in electrophysiology, pacemaker insertion, interventional cardiology and critical care medicine, and has won numerous awards as a teacher, researcher and educator. Dr. Bornstein’s long career working with cardiac pacemakers has paralleled the evolution of that technology.
PhysEmp CEO and Founder Robert Truog sat down with Dr. Bornstein for a far-ranging conversation about Dr. Bornstein’s life and work.
Bob Truog/PHYSEMP: You’ve been instrumental in working with pacemakers since the very beginning of the technology. I’d like to get your perspective on the recent technological advances. But first, give our readers a short primer on how pacemakers work.
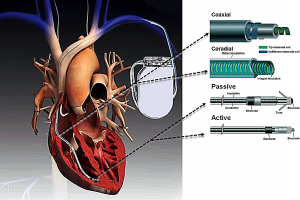
Pacemaker positioning and functioning
Dr. Bornstein: A pacemaker system primarily consists of a hermitically encased “can” that contains a battery as well as the circuitry. The can is connected to the cardiac muscle tissue by the pacemaker leads. The leads contain conductor coils that extend to the distal electrodes, which are separated by insulation material. The leads are primarily of coaxial design (a coil within a coil), following the configuration of the conductor coils.
PHYSEMP: How are the lead tips attached to the heart muscle tissue?
Dr. Bornstein: They’re attached by a penetrating helix, a design which is known as active fixation, or by tines that embed in the myocardial trabeculations, which is called passive fixation.
PHYSEMP: When was pacemaker technology first introduced?
Dr. Bornstein: Cardiac pacing was developed to produce electrical stimulation to initiate cardiac contractile activity. In the 1930s, Dr. Albert Hyman developed a device that used a hand crank to create an electric current. The current drove a DC generator whose electrical impulses were directed to the patient’s heart through a needle electrode placed percutaneously between the ribs into the heart muscle. At that point in history, neither the medical community nor society at large was ready to accept this kind of technology, which was deemed akin to sorcery.
PHYSEMP: Sorcery? No kidding?
Dr. Bornstein: It wasn’t until 1960, when Rune Elmqvist, an electrical engineer, and Dr. Ake Senning, a cardiac surgeon at the Karolinska Institute in Sweden, placed the first fully implantable pacemaker in a cardiac patient who had complete heart block and frequent syncopal attacks, or blackout spells.

PHYSEMP: In terms of your own interest in the field, what was it about pacemakers that first caught your attention?
Dr. Bornstein: I started with permanent pacemaker insertion as a cardiology fellow at Tufts New England Medical Center in 1974. At the time, the cardiovascular subspecialty of electrophysiology didn’t yet exist. As a matter of fact, the reason some physicians were training in electrophysiology was to get out of the draft for the war in Vietnam.
PHYSEMP: No kidding? How did that get them out?
Dr. Bornstein: It was because the subspecialty of electrophysiology was originally rooted in the Staten Island Public Health Service Hospital at that time; and so, if you were accepted into the training program, you were exempt from the draft. (As an aside, one of the pioneers in the field, Mark Josephson, M.D., who was one of the earliest developers of the subspecialty of invasive electrophysiology, spent two years at the Staten Island Public Health Service Hospital, an important training ground at that time for physicians interested in electrophysiology. He became recognized as an innovator of catheter-based treatment of cardiovascular dysrhythmias.)
PHYSEMP: So, in the early-70s, training in anything medically-related or public-health related got you an exemption?
Dr. Bornstein: Yes, but that wasn’t my situation. My family came to the United States in 1951 from postwar Germany, where I was born. The U.S. has just been incredible to me in terms of providing me with opportunities. I’ve lived the American dream. But back then, if I had gotten drafted, most likely I would’ve served as a medic, so I wouldn’t have to kill anyone. But I would’ve gone if called up. By the time I graduated medical school in 1973, however, the war was ending and we were in the process of withdrawal.
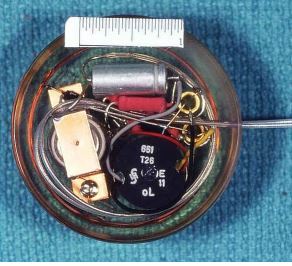
The first published report of the permanent implantable pacemaker. Reprinted with permission
from Surgery. Elmqvist R, Senning Å. Implantable pacemaker for the heart. In: Smyth CN, ed.
Medical Electronics: Proceedings of the Second International Conference on Medical Electronics,
Paris, 24–27 June 1959. London, UK: Iliffe & Sons; 1960:253–254
PHYSEMP: How did you first become interested in cardiology?
Dr. Bornstein: I chose invasive cardiology because it was the subspecialty that was the closest thing to surgery that I could find and yet still was deeply rooted in diagnostic medicine. I was also most interested in adult congenital heart disease which dealt with people who were born with congenital issues such as holes in their heart or were blue babies (cyanotic) and that sort of thing. They either had to have surgical correction or palliation. They were often underinsured because of their preexisting cardiovascular condition and underserved because of the complexity of their issues. I found them to be the most interesting patients having the most interesting clinical findings, which provided a large number of teachable moments.
PHYSEMP: When did you first start working with pacemakers?
Dr. Bornstein: I began training in pacemaker insertion during my three years of cardiology fellowship at Tufts New England Medical Center in Boston, 1975-1978. I did an extra year of training in cardiology at Tufts New England Medical Center where I trained in pacemaker insertion. At the time, we were one of the only fellowship programs in the country where you got to insert permanent pacemakers skin-to-skin in the cardiac catheterization laboratory without the involvement of a cardiac surgeon. Everywhere else, the procedures were always performed in an operating theater, often by a combination of a surgeon and cardiologist.
PHYSEMP: So at Tufts you actually performed all the surgery, including the incisions?
Dr. Bornstein: Yes. We did every aspect of the procedure. We created the pouch. We inserted the leads percutaneously through the subclavian vein, and under fluoroscopic guidance we positioned the leads determining the optimal pacing and sensing thresholds. We inserted the power pack subcutaneously under the skin. This was in the early to mid-1970s. A permanent pacemaker at that time was as big as a hockey puck. They had limited functionality, lasting approximately 1-2 years and harbored a host of technical problems. Today they are miniature electronic marvels.
PHYSEMP: What power source did you use in the early days?
Dr. Bornstein: The earliest power source we utilized were primarily mercury-zinc batteries in the early pacemakers. These were predicted by manufacturers to last 3-5 years but more often they lasted about a year or two at most. An alternative to the mercury-zinc battery, the nuclear generator, was conceived in the 1960s and brought to clinical fruition in the early 1970s. Obvious problems included the toxicity of nuclear exposure, the inordinate amount of paperwork, and the fact that the nuclear generator had to be retrieved postmortem and returned to the Nuclear Energy Commission. But by the mid-1970s, there was a new kind of pulse generator developed that combined lithium-based batteries, low current drain, and hermetic sealing as well as advanced circuitry.
PHYSEMP: So then every year or so you had to go in, cut, and put a new one in?
Dr. Bornstein: Exactly. It was easily accomplished because the leads previously inserted were still optimally functional. We just had to open the incision and replace the mercury-zinc battery. We did this until lithium iodide pulse generators became available. The lithium battery demonstrated a capability of functioning for 8-10 years.
PHYSEMP: Everything has obviously gotten much smaller, taking less and less energy to run. What was the next advance in the field?
Dr. Bornstein: The evolution of the field has been very interesting. The next advance was the lead-less pacemaker, which is what’s being developed now.
END OF PART I
Read Part II of this conversation